Note: The current recommended treatment is based on limited available information from current clinical data (Case-reports, published literature, Limited guidelines and expert opinion, Communicable disease Center-Qatar, CDC-USA, Up-to-date, Medscape), Internet book of critical care.
General Measures
- This treatment protocol is to assist physicians in management of patients with confirmed COVID-19 infection patients in order to guide the healthcare professionals.
- All therapies to the confirmed COVID-19 should be given with strict infection control measures as per your local needs.
- Samples (Both Oral/Nasal-Swabs) should be collected in negative pressure room (if not available single room with HEPA FILTERS)
- All healthcare staff should wear the full personal protective equipment PPE (Guan, gloves, N95 mask, face shield, eye protection whilst dealing with suspected/confirmed patients.
- All patients who are positive-COVID19, there swabs/PCR be repeated every 4-days till the test become negative.
- If the test of a suspected patient is negative for - COVID 19, then repeat after 24 hours.
- If 2 consecutive tests are negative, Isolation can be discontinued
- Lower respiratory specimen is preferred when applicable
- Airborne / contact isolation is recommended.
- Confirmed cases can be kept in same large room, if shortage of single isolation rooms
- keep in touch with your local Infection Control Team and follow their guidance.
- All patient should have their CBC, Urea & Electrolytes, CRP, Chest X-ray, Respiratory panel including COVID-19 PCR as a baseline investigation.
- Request G6PD level (as it may affect some of the medications given)
- Electrocardiogram (ECG), for all patients above 40 years of age.
- On clinical needs, request Bronchoscopy, CT Chest (if clinically indicated)
Definition of ARDS
- New or worsening respiratory symptoms within one week of known clinical insult.
- Chest imaging (X-ray/CT scan): bilateral opacities, not fully explained by effusions, lobar or lung collapse. Respiratory failure not fully explained by cardiac failure or fluid overload.
- Mild ARDS: 200 mmHg < PaO2/FiO2 ≤ 300 mmHg (with PEEP or CPAP ≥5 cmH2O, 7 or non-ventilated)
- Moderate ARDS: 100 mmHg < PaO2/FiO2 ≤200 mmHg with PEEP ≥5 cmH2O, 7 or non-ventilated)
- Severe ARDS: PaO2/FiO2 ≤ 100 mmHg with PEEP ≥5 cmH2O, 7 or non-ventilated)
- When PaO2 is not available, SpO2/FiO2 ≤315 suggests ARDS (including in non-ventilated patients)
Treatment
- Admit the patient Hospital
- Chloroquine phosphate 250 mg (150 mg base )300 mg (base) BID or Hydroxy Chloroquine 400 mg OD, Orally for 10-days
PLUS - Oseltamivir 150 mg BID, Orally for 10-Days.
PLUS - Darunavir /Cobicistat) (Rezolsta ®) Darunavir 800 mg/Cobicistat 150 mg OD for 2 weeks
OR - Ritonavir + Lopinavir (Kaletra) 500 mg BID for 2 weeks
PLUS - Azithromycin + IV (as per local guidelines for community acquired Pneumonia)
- And/Plus Consider ( In very high risk patients)…… See below
- Convalescent Plasma Infusion (2 units of CP. Each unit of plasma (200 -250 ml) will be given over 2 h with an interval of 1 h between the two units)
Plus Consider - Methylprednisolone 40 mg IV BID for 5 days
PLUS (may consider in severe cases, ****** under investigations (follow local Guidance) - Tocilizumab for patients with evidence of cytokine release syndrome IV, (IV infusion: initial dose of 4–8 mg/kg infused over more than 60 minutes. If initial dose not effective, may administer second dose (in same dosage as initial dose) after 12 hours. No more than 2 doses should be given; maximum single dose is 800 mg and not to be infused in the same line with other medications) *****
Steroid use
- Intravenous glucocorticoid therapy should not be used as initial therapy
- Should be considered on a case-by-case, for selected patients with refractory shock (defined as a systolic blood pressure &It;90 mmHg for more than one hour following both adequate fluid resuscitation and vasopressor administration).
Treatment - Respiratory Support

- Non-invasive respiratory support
- Low flow Nasal Canula: typically, 1-6 liters/minute
- High Flow Nasal Cannula:
- front-line approach to noninvasive support
- This typically requires less maintenance than invasive mechanical ventilation
- Keep between 15-30 liters/minute.
- Noninvasive ventilation (BiPAP)
- Probably isn't useful for most patients
- Viral filter should be placed in-line with the exhalation tubing to reduce environmental contamination.
- BiPAP using a helmet interface may be considered
Intubation Procedure
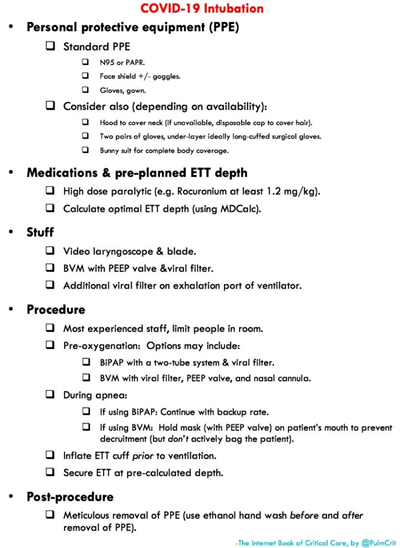
Invasive Mechanical Support
- What type of ARDS caused by COVID?
- COVID doesn't appear to cause substantially reduced lung compliance (which is generally a hallmark finding of ARDS).
- The predominant problem might be one or more of the following (based on current research)
- Atelectasis (alveolar collapse)
- Drowning of the alveoli by fluid
- If atelectasis, then this will be relatively easy to manage. Any strategy to increase the mean airway pressure will treat atelectasis (e.g. APRV or conventional ARDS net ventilation using a high-PEEP strategy).
- If drowning of the alveoli: this is usually very difficult to manage.
- Proning may facilitate drainage of secretions.
- APRV may also be useful to facilitate airway clearance (rapid dumping breaths create expiratory airflow that can facilitate secretion clearance).
- Conventional ARDS Net Ventilation
- Tidal volumes should be targeted to a lung-protective range (6 cc/kg ideal body weight).
- High PEEPs should be utilized.
- An ARDSnet “high PEEP” table is shown below (guidance only-tailor according to your need)

Renal Support
- Renal failure requiring dialysis has been reported in patients admitted to ICU.
- Rhabdomyolysis may contribute to acute renal failure.
- Patients who develop renal failure has a poor overall prognosis.
ECMO (Cardio-Pulmonary Support)
- This decision depends on clinical status, local resources and capabilities, patient age and related comorbidities.
- If younger patient, and suffering from single-organ failure due to a reversible etiology, so many would be excellent candidates for ECMO.
- VV ECMO could be used for respiratory failure
- VA ECMO could be useful in patients with fulminant cardiomyopathy and cardiogenic shock